Overview
A large not-for-profit human services agency, providing a variety of behavioral and mental health and developmental disabilities services through a diverse set of programs through its network of facilities that includes residential housing, shelters and clinics, embarked on a strategic mission to improve care delivery through technology-enabled transformation. To jump-start this process, the organization engaged RSM’s health care technology and management consulting team to perform an evaluation and selection of an electronic health record (EHR) platform that aligned with the organization’s goals and its vision, unifying workflows and replacing its legacy system.
Business concerns
Industry challenges
Behavioral health has long been on the periphery of health care because of prevalent reimbursement models, regulations and the cultural stigma associated with behavioral and mental health issues. This is changing dramatically due to a renewed interest in taking care of the whole person, from a physical and mental health perspective, and with growing literature that endorses the importance of addressing social and behavioral determinants of health when caring for an individual via an integrated health, value-based care or population health management paradigm.
With a greater focus on the behavioral and mental side, organizations that provide these services need to chart a road map to modernize their operations and their use of technology to enable care transformation that makes it possible to measure, benchmark and improve from a quality improvement and cost containment perspective.
Care transformation, enabled by technology modernization, within these organizations requires a substantial amount of focus. Unfortunately, the vendor landscape for behavioral health EHRs has yet to mature with respect to functionality and services. As a result, when it comes to care documentation, billing and regulatory reporting, a fragmented best-of-breed approach, as opposed to an integrated enterprise approach, is prevalent within the industry.
Inefficiencies and inconsistencies in communication between these systems lead to poor adoption and ultimately a poor return on investment from a technology and resources perspective. Ultimately, the goal of being able to document effectively and share that data with outside entities such as health information exchanges, accountable care organizations, referring providers, or affiliated hospitals is left unrealized.
While these challenges may seem consistent with what is seen on the physical health side, or even with other industries that are making a transition to digital, there are some unique challenges specific to the behavioral health industry, including clinical and financial workflows, reporting requirements, and the sensitivity of patient information.
Additionally, the standardization in care delivery is at a nascent stage at the moment. In addition, vendors have vastly different capabilities. A strategic approach to identify technology needs, and an EHR system, is essential.
Organizational challenges
The client’s current EHR had proven to be a burning platform, with significant organizational angst. They indicated the following concerns and issues:
- Consensus building was needed with respect to a new EHR platform across the organization and its varied service and program verticals.
- An EHR vendor needed to be identified that was a cultural fit for the organization.
- The need to utilize standard content versus building new would need to be balanced within the new EHR.
- For consumer assignment, quality and regulatory reporting, third-party data integration was needed with city and state agencies that used antiquated IT systems.
- Intake forms, assessments and treatment plans across all programs required integration.
- Billing efficiencies required improvement through a clinical documentation-driven integrated workflow.
- Transition plans for legacy data from paper and electronic data in the current state to the new platform was needed.
- IT resources required allocation to support operational activities while implementing a new EHR system.
- Financial implications needed to be considered with sun-setting an old system and investing in a new one.
Our approach
Highlights from RSM’s EHR selection methodology to help the client included the following:
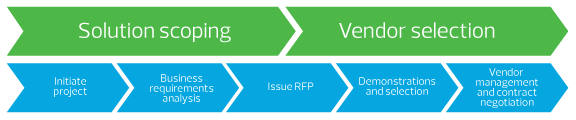
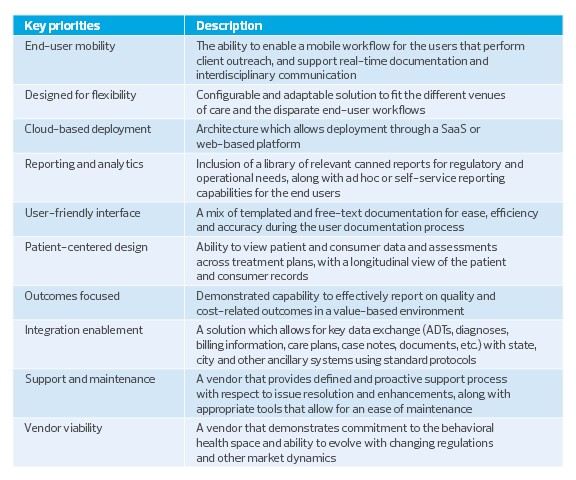
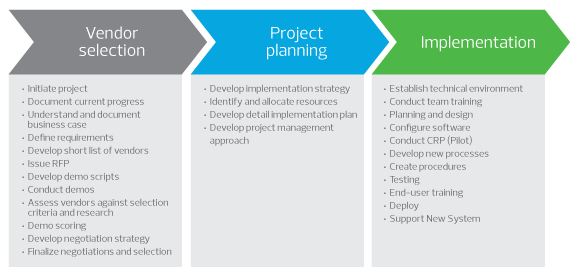
1. Solution scoping and vendor selection. Through a defined solution scoping and vendor selection approach, an area of primary focus was established. Guiding principles and key priorities for the organization were articulated. Formulating these criteria required building consensus within the organization and developing an objective methodology for selection. The following graphic illustrates the plan.